JEAVONS SYNDROME: Uncommon but not Unseen
Introduction
Epilepsy, an ancient medical condition dating back to 4000 BCE, has long been shrouded in stigma and misunderstanding, affecting the quality of life for individuals and their loved ones. This disorder, characterized by unprovoked seizures, affects people of all ages, with a particular inclination toward the very young and the elderly.
Among the various forms of epilepsy, Epilepsy with Eyelid Myoclonia (EEM), formerly known as Jeavons Syndrome, remains relatively rare and often misdiagnosed or underdiagnosed. In 2017, the International League Against Epilepsy (ILAE) officially recognized EEM as a distinct diagnosis, referring to it as “absences with palpebral myoclonus.” The ILAE neurophysiology task force subsequently outlined the unique clinical and electroencephalographic (EEG) features that characterize EEM.
Demographics
EEM affects approximately 2.5% to 2.7% of all epilepsy cases, with a higher prevalence among females, accounting for 7.3% to 12.9% of all generalized epilepsies. Typically, seizures associated with this syndrome begin between the ages of 6 and 8, with a peak occurrence between 2 and 14 years. However, identifying the exact onset of seizures can be challenging, as eyelid twitches may be mistaken for tics or mannerisms, and absences may go unnoticed. A notable 33% to 83% of cases exhibit a family history of epilepsy, suggesting a genetic component.
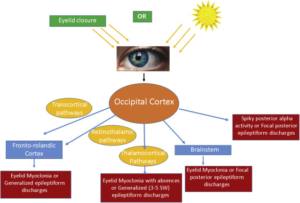
Pathophysiology
Clinical Features
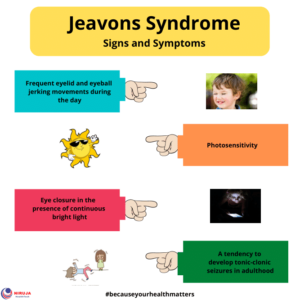
EEM is characterized by a hallmark electroclinical triad, including:
1. Eyelid myoclonia with or without absences
– These involve brief, repetitive myoclonic jerks of the eyelids immediately after closing the eyes, often accompanied by a brief 3-6 Hz spike and wave activity.
– The eyelid movements resemble rapid blinking, with the eyes deviating upwards, distinguishing them from the slight flicker of eyelids in typical absence seizures.
– These events are typically brief, lasting less than 6 seconds, but can occur frequently throughout the day. They are often triggered by eye closure, flashing lights, or exposure to television or video games.
– When accompanied by a brief loss of awareness, the seizure is termed “eyelid myoclonia with absence.” In some cases, individuals can experience eyelid myoclonic status epilepticus, where eyelid myoclonia and absences occur back-to-back over an extended period.
2. Generalized tonic-clonic seizures are less common and primarily occur in older children and adolescents. They are often provoked by factors such as sleep deprivation or light stimulation.
3. Myoclonic jerks of the arms and legs may occur but are infrequent.
Individuals with Jeavons Syndrome may receive misdiagnoses during childhood, with eye fluttering mistakenly attributed to tics or other forms of epilepsy. Consequently, this condition may go undiagnosed until adulthood, when eyelid myoclonia becomes more pronounced and affects daily life significantly.
Diagnosis
Diagnosing Jeavons Syndrome typically involves several key approaches:
1. Extended duration video electroencephalogram (EEG)
– Repeatedly closing and opening the eyelids triggers transient bursts of high-amplitude activity, characterized by fast generalized 3-6 Hz polyspike and wave patterns lasting 1-6 seconds.
– Prolonged eye closure results in increased alpha frequency activity that extends to frontal areas.
– Photoparoxysmal discharges induced by photic stimulation are common in untreated young patients.
– Hyperventilation may also provoke abnormal EEG patterns.
Electroencephalography of an absence seizure with eyelid myoclonia in Jeavons syndrome:
– The absence seizure is triggered by eye closure, characterized by paroxysms of generalized, fast polyspike activity.
– Interictal generalized polyspike-wave discharges during sleep can also be recorded.
2. MRI scan is often performed to exclude brain abnormalities, although results are typically normal.
3. Genetic testing may yield positive findings, further supporting the underlying genetic etiology of the syndrome.
Differential Diagnosis
Jeavons Syndrome should be distinguished from various conditions, including:
– Facial tics
– Conditions with eye closure sensitivity (e.g., juvenile absence epilepsy, juvenile myoclonic epilepsy, idiopathic occipital lobe epilepsy)
– Conditions associated with eyelid myoclonia (e.g., childhood absence epilepsy, juvenile absence epilepsy, and sunflower syndrome)
– Photosensitive seizures (e.g., benign myoclonic epilepsy of infancy, idiopathic generalized epilepsy with tonic-clonic seizures, and Dravet’s syndrome)
Treatment
Managing Jeavons Syndrome involves both pharmacological and non-pharmacological approaches:
1. Anti-seizure medications are a primary treatment modality. Valproate, often in combination with clonazepam, levetiracetam, lamotrigine, or ethosuximide, has shown efficacy, with the choice of drug depending on the main seizure type.
– Clonazepam is highly effective against eyelid myoclonia and myoclonic jerks.
– Levetiracetam is effective due to its anti-myoclonic and anti-photosensitive properties.
– Lamotrigine can help manage absence seizures but may worsen myoclonic jerks.
2. Non-pharmacological treatments include:
– Photoparoxysmal avoidance: Using special glasses with blue Z1 lenses to prevent photic triggers.
– Modified Atkins diet: High in fats, proteins, and limited in carbohydrates, it can be effective, especially for photosensitivity.
– Vagus Nerve Stimulation (VNS) Therapy: An FDA-approved treatment that involves implanting a device under the skin to deliver regular, mild electrical pulses to the brain via the vagus nerve. VNS therapy has been shown to help control seizures in Jeavons Syndrome patients by increasing blood flow to the brain, modulating neurotransmitter levels, and altering EEG patterns.
Vagus Nerve Stimulation (VNS) Therapy:
– The device is implanted in the left chest area, with an electrode/wire attached to the vagus nerve in the neck.
– Regular stimulation can be enhanced during a seizure by swiping a magnet over the device in the chest area.
Conclusion
Jeavons Syndrome, now recognized as EEM, is a rare and often misdiagnosed form of epilepsy with distinct clinical and EEG features. Early diagnosis and appropriate treatment, whether through medication or non-pharmacological interventions, can significantly improve the quality of life for individuals living with this condition. Awareness and understanding of Jeavons Syndrome are crucial steps towards providing better care and support for those affected.
References
1. Kuriakose ME, Zacharias R, Athira R353 Jeavons syndrome-a photosensitive epilepsy syndrome. *Archives of Disease in Childhood*, 2022;107:A220-A221.
2. Zawar et al. *Epilepsy With Eyelid Myoclonia (Jeavons Syndrome)*.
3. Seneviratne, Udaya & Cook, Mark & D’Souza, Wendyl. Electroencephalography in the Diagnosis of Genetic Generalized Epilepsy Syndromes. *Frontiers in Neurology*, 2017. 8: 499.
4. Yujun Yuan et al. Case Report: A Case of Eyelid Myoclonic Status With Tonic–Clonic Seizure and Literature Review.
5. Seizure Devices – Vagus Nerve Stimulation (VNS) Therapy – Epilepsy.com.
6. Nirujahealthtech.com.
CLICK HERE TO BUY OUR FIRST EDITION OF MAGAZINE AT FLAT 25% DISCOUNT USE CODE “MAGAZINE”
NOW AVAILABLE ON AMAZON

Written By: Dr. Akanshi Oberoi, MBBS, Government Medical College, Patiala, Punjab
